

Featured
Corporate Wellness
Medication for Weight Loss: Not an Instant Solution
Who is a candidate for the newly approved drugs and are they effective?
Corporate wellness articles that deliver physical, behavioral, and well-being information for healthy employees and business.

Corporate Wellness
BeneQUIT Helps Two Colleagues Kick Smoking Habit
January 19, 2024
Kicking the habit is one of the greatest and most rewarding challenges a smoker can face.

Executive Health
Executive Health
January 11, 2024
A concept that taps into longevity, prevention, cost-savings, convenience, and more.

Behavioral Health
Coping with Financial Stress
December 13, 2023
The reasons for the stress vary and it's important to understand the psychological factors that shape our response.

Corporate Wellness
Medication for Weight Loss: Not an Instant Solution
November 20, 2023
Who is a candidate for the newly approved drugs and are they effective?


Corporate Wellness
Why Are We Too Tired to Get Healthier?
August 22, 2023
If you have an energy deficit, it is more challenging to step up physical activity or change your diet – two basic steps to a healthier lifestyle.

Behavioral Health
Total Well-Being and its Rewards for Employers
July 17, 2023
Happy employees equal a stronger, potentially more profitable business.

Fitness
The Evidence Stacks up on Physical Activity: It’s a Must for Health
June 6, 2023
Sedentary behaviors in the office, watching TV, and scrolling screens are terrible for our health. Here are quick tips, top facts, and motivation to help.

Corporate Wellness
Total Well-Being Transcends Your Plan
June 1, 2023
How one business executive got healthier by building on his company’s insurer-provided wellness offerings.

Corporate Wellness
Expanding Care Beyond the Physician
May 15, 2023
Care teams give patients an added layer of attention, expertise, and peace of mind

News
Populytics Focuses on Total Well-Being with New Website
May 3, 2023
New site showcases the company’s expanded direction for employer groups

News
Four New Directors Announced in Populytics Technology Sector
March 20, 2023
With a history of data analytics expertise, strong leaders will head up analytics, engineering, and clinical and business intelligence

Health Insurance
How Primary Care Physicians Help Employers
February 28, 2023
Preventive health care is so essential to keeping ourselves from becoming chronically sick in the future

Corporate Wellness
Help Your Employees Get Back on Track with Health Coaching
January 10, 2023
Coaches help employees set goals, then support and motivate to help achieve them

News
Health Coach/Tobacco Cessation Specialist Christine Lanasa Earns LVHN’s Proud Partner Award
November 7, 2022
The award is given to those employees who have exemplified LVHN Core Values toward colleagues, patients, and families.

Fitness
Let the Change of Seasons Inspire Good Health with Fall Activities
October 28, 2022
Connect with the beauty of the changing landscape and feel an emotional boost

Health Insurance
The Well-Being Factor is Changing Employer-Sponsored Health Care Forever
October 5, 2022
Preventive health care and well-being for employees lowers costs for companies

Health Insurance
What is Value-Based Care and Why is it Important for Employers to Understand it?
August 4, 2022
A different approach and plan solution to match

News
Robert X. Murphy Jr., MD and Tom Marchozzi Assume Top Leadership at Populytics
July 26, 2022
Populytics announces reorganization and new leadership

Health Insurance
High-Value, Simplified Health Care Options for Employers
June 20, 2022
How one population health management firm’s advanced analytics paved the way.

News
Michael J. Weiss Named Administrator of Informatics at Populytics, Inc.
June 10, 2022
With LVHN for 15 years, he has taken on increasing responsibility across the enterprise, specifically focused on research and business functions.

Behavioral Health
Mental Health at Work: It’s Time for Openness and Acceptance
May 18, 2022
Three steps recommended to begin building a culture of mental health support

News
Business Development Team Expands With Direct-To-Employer Health Care Sales Specialist
May 6, 2022
Zackary Jones has joined the Business Development, Sales, and Marketing Team as Sr. Sales Executive.

Behavioral Health
Why Employers Should Focus on Employee Wellness
March 29, 2022
We spend one-third of our lives working, how companies create workplaces that support our health has a huge impact on our overall wellness.

News
Denise Woodworth Among Lehigh Valley Business “Women Of Influence”
March 29, 2022
Honorees have been selected based on tremendous professional accomplishments, community involvement, and a commitment to mentoring

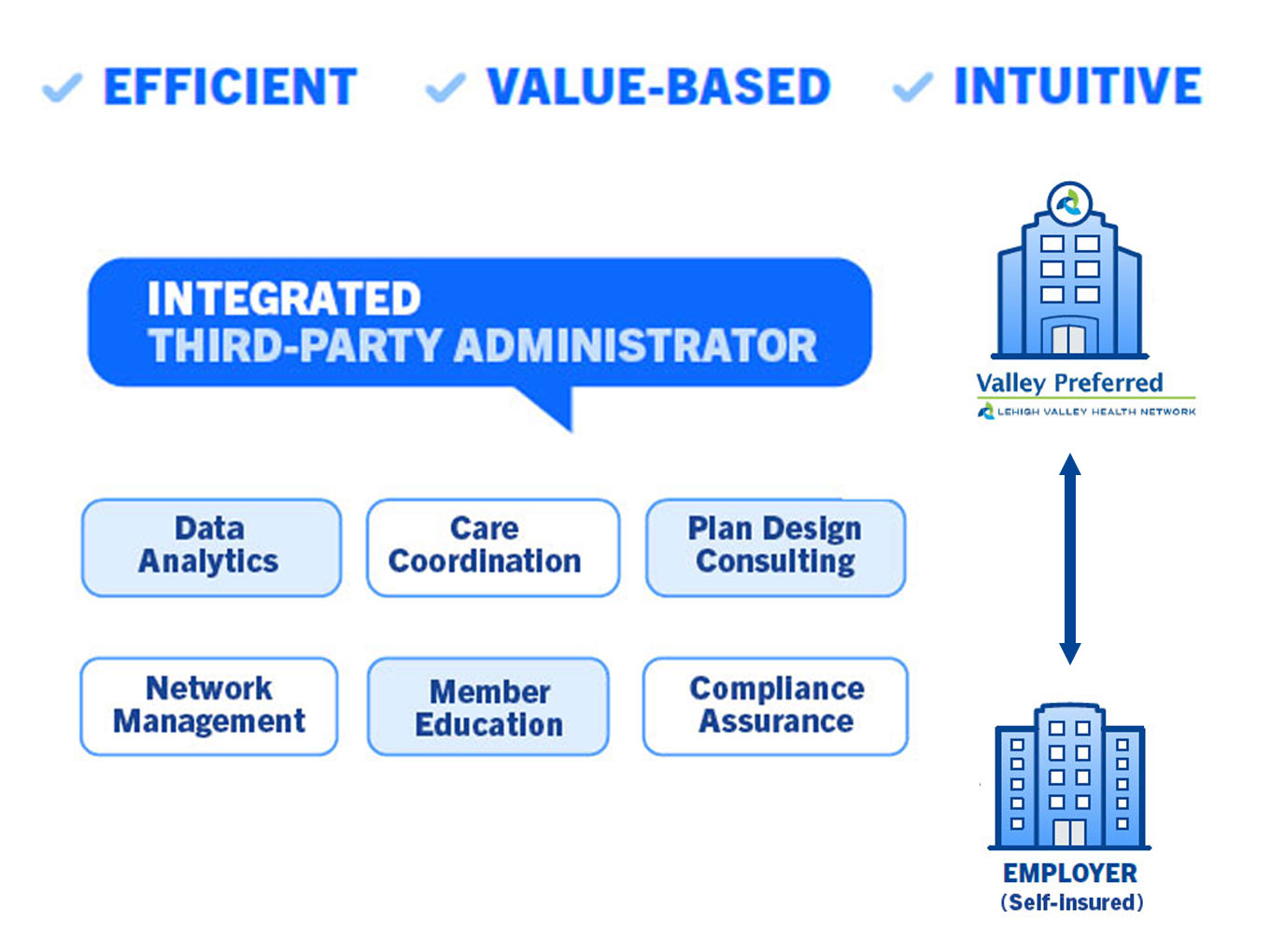
Health Benefits Administration
Why Companies Like GM & Walmart Opt for Direct Health Care Contracting
March 15, 2022
The alternative approach on how taking charge can mitigate health insurance costs & offer better benefit designs and offerings for employees

News
Carol Michaels Named President-Elect of ACHE of Eastern Pennsylvania
March 8, 2022
Carol Noel Michaels, Administrator of Care Coordination at Populytics named President-Elect of the PA American College of Healthcare Executives (ACHE) for 2023.
Health Insurance
Integrated Third-Party Administrator Can Improve Health Plan Value
February 3, 2022
Self-insured health care plans have grown in popularity in response to changes in the market

News
Populytics is Keeping the Momentum Going with New Sales Executive
January 24, 2022
Populytics has added seasoned sales professional Cary Salkin to its business development team to further promote its comprehensive well-being portfolio.

Executive Health
LVHN Aims for Convenience with Executive Health Program
January 5, 2022
Personalized medical exam and screening program for time-pressed executives, working moms and dads. One day convenience in private suite.
Health Insurance
What is Direct Health Care Contracting?
December 14, 2021
Self-insured employers can have direct arrangements with providers which can create innovative cost controls and address workforce needs.

News
Populytics Energizes Sales and Marketing with New Administrator
December 9, 2021
Populytics welcomes Bob Knauss, Admin., Business Development, Sales and Marketing, who will create sustained awareness and application of our services.

Corporate Wellness
Building a Healthy Hybrid Team
September 14, 2021
5 elements for merging remote, hybrid, and in-person work cultures

Behavioral Health
Empathetic Leadership, a Must-Have in Today’s Workplace
August 23, 2021
Empathetic leaders can see their employees as a company’s greatest asset and take responsibility for the well-being and success of the group.

Behavioral Health
Back to Basics in Mental Health
June 16, 2021
Workplace settings with significant “companionate love” have a positive effect on the emotional well-being of employees. So what is that?

Behavioral Health
3 Steps to Keeping Workday Stress at Bay
April 27, 2020
In today’s hyperconnected world, the ease of multitasking has resulted in an "always-on" culture. Find out the best ways to manage stress in the workplace.

Corporate Wellness
Employee Tobacco Cessation Delivers Significant Savings
February 25, 2020
Employers can save $6,000 per year for every employee who quits smoking. Five ways to reinforce a “quit” culture, and how to identify a successful program.

Behavioral Health
Mindfulness as a tool in the modern-day workplace
January 30, 2020
With 83% of U.S. workers suffering from work-related stress, mindfulness is an easy-to-learn practice that is linked to lower emotional exhaustion.

Corporate Wellness
What you Need to Know about e-Cigarettes
October 25, 2019
E-cigarettes have addictive nicotine. CDC has issued a health advisory after an outbreak of severe lung disease. Learn how to quit and find resources.

Corporate Wellness
A Wake-Up Call About Sleepiness and Fatigue at Work
June 17, 2019
Millions of Americans do not get enough sleep, which can have a significant effect on your health, safety, productivity and quality of life. Learn more.
Fitness
Choose Your Own Fitness Path
June 14, 2019
The best way to work toward healthy habits, such as regular exercise, is to set goals aligned with what you value.

Corporate Wellness
10 Habits to Maintain Good Health
August 18, 2018
We need to maintain good health if we want to be and stay healthy. Here are 10 powerful habits that you can use to improve your health.

Behavioral Health
Addressing Employee Alcohol and Drug Issues
July 24, 2018
Our Employer Assistance Program helps identify and intervene appropriately with employees who may be using substances at work.
Health Insurance
What are Tiered Health Insurance Plans?
April 6, 2017
Businesses with employer-sponsored health plans want access to high-quality providers that don’t break the bank. Learn about tiered health insurance plans.

Corporate Wellness
Slipping on Your Wellness Routine? How to Stick to it.
March 20, 2017
Slipping on your wellness routine is not the end of the world. Here's how to keep a lapse from becoming a relapse.

Behavioral Health
Resilience: How to Increase your Ability to Cope with Difficulties
February 16, 2017
Nurturing one particular quality can help increase your ability to cope in and out of work.

Health Benefits Administration
4 Steps to Data-Driven Business Development
December 18, 2016
Learn about data collection, modeling, visualizing, and discovery.

Corporate Wellness
Two easy steps to start a successful workplace wellness program
September 21, 2016
To get started on a new corporate program, determine where you're beginning. These steps can ensure a better chance of success.
Corporate Wellness
5 Questions When Choosing a Corporate Wellness Provider
March 30, 2016
Ask about the background, education, training and certifications of the wellness team with whom you and your employees will be interacting.